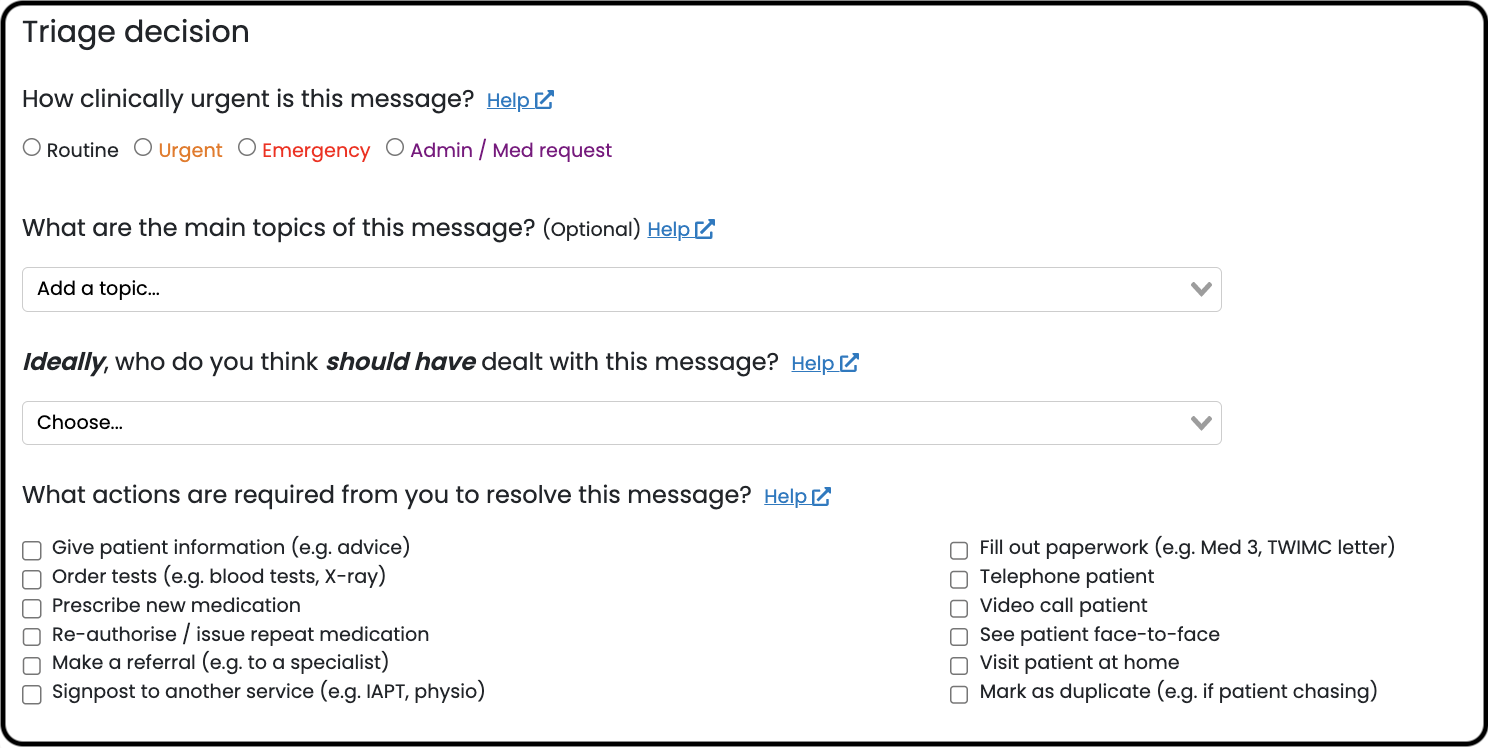
There are four triage decision questions:
- How clinically urgent is this message?
- What are the main topics of this message?
- Ideally, who do you think should have dealt with this message?
- What actions are required from you to resolve this message?
Why do we collect triage decisions?
- To prioritise your inbox and improve patient safety. Adding an urgent or emergency triage decision applies an orange / red flag and sends the request to the top of the inbox so you and your colleagues know which requests need attention first. Triaging a request as an admin or medication request applies a purple flag and sends it to the bottom of your inbox so you know you can deal with it later.
- To collect important data for your Patchs reports. All your practice triage decisions are available for you to view in your Practice Reporting Dashboard, so you can track what you and your staff have done with each request. You can use this data to evaluate your own practice performance and patient demand, e.g. how many Patchs requests have a required a face-to-face appointment or telephone call, how many should have been sent somewhere else, or what type of clinical topics they presented with. This can be helpful to plan your capacity and the skill mix of staff you may need.
- To teach Patchs AI to triage and workflow requests on its own. Patchs AI uses machine learning, meaning that each time you triage a patient request you're teaching it what to do with similar requests in future. Patchs AI can flag requests as urgent or emergency, signpost patients away when appropriate, ask patients further questions about their request, assign requests to clinicians, and highlight if a request may need a face-to-face consultation - thereby reducing your workload and increasing patient safety.
- To monitor how Patchs AI is performing. As a Class I Medical Device we continually monitor the performance of Patchs AI to ensure it is safe and see if it could be improved. We do this through the triage decisions you make - in particular decisions made by clinicians.
When a request needs clinical input, assign the request to a clinician to make the triage decision
When a non-clinical member of staff (e.g. receptionist) thinks a request needs a clinician to deal with it, they should assign the request to a clinician within Patchs so they can add their triage decision. We recommend they do not save the request to the clinical record themselves and book in the patient for a telephone or face-to-face appointment with a clinician because:
- It can decrease workload. Clinicians may be able to signpost some patients to pharmacy / self-care, A+E, or other providers (e.g. first contact physio) without conducting a telephone or face-to-face consultation. Non-clinicians may not have the confidence or knowledge to do this. So it can save resources rather than booking-in patients directly for telephone or face-to-face appointment.
- Clinicians benefit from an all-in-one system. If clinicians choose to consult the patient, either straight away or on a future date (e.g. using the booked slots feature), they get the benefits of using Patchs including easily replying to patients with written messages, video consultations, clinical questionnaires etc - you don’t have to use separate systems to do each thing.
- It doesn't clog up the patient record. If you send patients messages when replying to their request, it's saved to their record as one consultation. If you use a separate messaging system to reply, each message may be saved as a separate consultation, which clogs up the patient record.
- It's better for teaching and monitoring Patchs AI. Because Patchs AI makes clinical decisions, triage decisions made by clinicians are primarily used to teach and monitor it, rather than triage decisions from non-clinical staff (although we do use triage decisions made by non-clinical staff when they don’t need clinical input).
Make triage decisions straight away and update them later
We recommend making triage decisions as soon as you read a request based on what you think you may ultimately do with it, not necessarily what you're doing with it right now. For example, if you think the request may end up with a telephone or face-to-face consultation you should triage it as so. You can then update your triage decision if you get more information from the patient. This is because:
- It's safer. As mentioned above, marking a request as urgent or emergency applies an orange / red flag and sends it to the top of the inbox, and marking one as an admin or medication request applies a purple flag and sends it to the bottom of the inbox. This enables both you and your colleagues to know which requests need attention first. This is especially important if you assigning the request to someone else, e.g. if the request needs input from a clinician. The sooner you make the triage the decision, the sooner this information is available.
- It allows you to remove the request from your inbox. If you want to remove the request from your inbox, you can only do this if the triage decisions are completed. You may want to do this if: 1) you're waiting for a patient to reply to a message you've sent and don't want the request hanging around in your inbox, 2) you've added a task for someone else and don't want the request hanging around in your inbox, 3) you've completed the request.
- It's better for teaching and monitoring Patchs AI. Patchs AI works as soon as requests are submitted by patients, so adding triage decisions straight away means you're teaching and monitoring Patchs AI the job it's meant to do. If you only add your triage decisions later when you have more information from the patient, this isn't as useful for teaching and monitoring Patchs AI.
If you're going to assign the request to someone else (for example if you're a receptionist and the request needs input from a clinician) then we recommend only completing the first triage decision question about clinical urgency (How clinically urgent is this message?).
The questions
1. How clinically urgent is this message?
Your answer should relate to the clinical urgency of the request. The options are:
- Routine: Patient unlikely to be harmed if this request is not resolved within the next 48 hours.
- Urgent: Patient could be harmed if this request is not resolved within the next 48 hours.
- Emergency: Patient could be harmed if this request is not resolved on the same day. May require emergency services.
- Admin / Med request: Administrative or medication request.
Requests marked Urgent or Emergency are sent to the top of the inbox. Those marked Admin / Med request go to the bottom.
It's important you make your decision purely based on the clinical urgency of a request. For example, you shouldn't mark requests urgent just because a patient is chasing a response about a non-urgent request they haven't received a reply about yet.
2. What are the main topics of this message? (Optional)
This refers to what is written by the patient in their request. The full list of topics to choose from is here and we are always adding more.
Some topics may already be added by Topic AI. Please delete those you think aren't relevant, and add any you think are missing.
3. Ideally, who do you think should have dealt with this message?
You should only answer this question if you're going to complete the request, not if you're going to assign it to someone else to deal with.
You should answer this question in terms of what should happen in an ideal world if this same request was submitted again in future. For example:
- You're a GP. The patient has athlete's foot which they could have had treated at a pharmacy, but you gave them a prescription for anti-fungal cream anyway. You should choose 'Pharmacist outside my practice (e.g. minor ailments scheme)'.
- You're a receptionist. The patient has chest pain and you advised them to go to A&E but they refused and asked to speak to a GP instead. You assigned the request to a GP to deal with urgently. You should choose 'A&E / 999'.
It doesn't matter if you don't have a particular service nearby, like a pharmacist that can deal with minor illnesses, you should answer what should happen in an ideal world.
The options to choose from are:
- Patient themselves (e.g. self-care). The request should not have been submitted to your practice at all, and the patient could have instead resolved the request on their own.
- Pharmacist outside my practice (e.g. minor ailments scheme). The request should not have been submitted to your practice at all, and the patient could have instead gone to a pharmacist to resolve their request.
- A&E / 999. The request should not have been submitted to your practice at all, and the patient should have instead gone to A&E or called 999.
- Dentist. The request should not have been submitted to your practice at all, and the patient should have instead gone to the dentist.
- Receptionist.* A receptionist could have resolved the request, but you have dealt with it anyway.
- Pharmacist inside my practice.* A pharmacist could have resolved the request, but you have dealt with it anyway.
- Secretary.* A secretary could have resolved the request, but you have dealt with it anyway.
- Nurse.* A nurse could have resolved the request, but you have dealt with it anyway.
- Advanced practitioner.* An advanced practitioner could have resolved the request, but you have dealt with it anyway.
- Physiotherapist. A physiotherapist could have resolved the request, but you have dealt with it anyway.
- OOH service (including NHS 111) The request should not have been submitted to your practice on this occasion and the patient should have instead used an OOH service, including NHS 111
- Me. You are the right person to resolve the request. You should only choose this option if you are clinically the most appropriate person to resolve the request. If you are a receptionist and the patient requires input from a clinician, you should not choose this option. Instead you should assign the request to a clinician to deal with in Patchs.
4. What actions are required from you to resolve this message?
You should only answer this question if you're going to complete the request, not if you're going to assign it to someone else to deal with.
You should select as many actions as you think are relevant to resolve the request.
The options for clinical staff are:
- Give patient information (e.g. advice)
- Order tests (e.g. blood tests, X-ray)
- Prescribe new medication
- Re-authorise / issue repeat medication
- Make a referral (e.g. to a specialist)
- Signpost to another service (e.g. IAPT, physio)
- Fill out paperwork (e.g. Med 3, TWIMC letter)
- Telephone patient
- Video call patient
- See patient face-to-face
- Visit patient at home
- Mark as duplicate (e.g. if patient chasing)
The options for non-clinical staff are:
- Give patient information (e.g. advice)
- Issue medication (e.g. repeat)
- Signpost to another service (e.g. pharmacy, DNs, physio)
- Book pre-agreed appointment (e.g. blood test, smear, decision by GP). This option should only be used to book a GP appointment after a GP has assigned a triage decision saying they need an appointment.
- Chase something (e.g. results, referral, prescription)
- Telephone patient
- Mark as duplicate (e.g. if patient chasing)
Triage decision frequently asked questions
Why are some options only visible to clinicians?
For example, for the triage question 'ideally, who do you think should have dealt with this message?', non-clinicians do not see the options 'nurse' or 'advanced practitioner'. For the triage question 'what actions are required from you to resolve this request?', non-clinicians do not see the options 'video call patient', 'see patient face-to-face', or 'visit patient at home.
This is because these triage questions should only be answered if you have completed the request (not if you're going to assign it to someone else to deal with). And because these are primarily clinical decisions, they should only be made by clinicians.
I've given advice to a patient - what options should I choose?
If you've given advice that only you could give (e.g. you're a GP and you've given reassurance or self-management about a potentially serious condition), you should select 'me' for 'ideally, who do you think should have dealt with this message?' and 'give patient information (e.g. advice)' for 'what actions are required from you to resolve this request?'.
If you've given advice to a patient for something they should have got treated elsewhere, e.g. a minor illness that they could have gone to a pharmacist about, you should select 'pharmacist outside my practice (e.g. minor ailments scheme)' for 'ideally, who do you think should have dealt with this message?' and 'give patient information (e.g. advice)' or 'signpost to another service (e.g. IAPT, physio)' for 'what actions are required from you to resolve this request?'.
A patient is chasing a response for something that's not urgent, should I mark it as urgent?
Ideally not because the triage decisions should be made on clinical grounds.
What should I do if the exact action I want to take with this request isn't available?
We have developed and refined these triage decisions based on feedback from hundreds of practices that have triaged hundreds of thousands of requests. We are confident that almost all triage decisions are captured in the available options. Some specific examples:
- You've asked the patient for photographs or for further information. As mentioned above, you should make triage decisions early based on what you think you may ultimately do with a request, not necessarily what you're doing with them right now e.g. if you think the request may end up with a telephone or face-to-face consultation you should triage it as so.
- You've asked the patient to contact the surgery to make a telephone or face-to-face appointment. You should choose 'telephone patient' or 'see patient face-to-face'.
- The patient has just given us some information e.g. a progress report or feedback. You should choose 'give patient information (e.g. advice)'.